Research body making important strides in the study and development of best practices for adaptive radiotherapy
In April 2019, Varian announced the formation of the Adaptive Intelligence™ Consortium (AIC), a global community of clinicians and scientists from leading cancer clinics working to develop best practices for adaptive radiotherapy based on clinical evidence. In September that year, Varian introduced Ethos® therapy, an AI-driven solution designed to enable clinicians to adapt a patient’s treatment plan each day based on tumor and anatomical changes and deliver the treatment within a typical 15-minute timeslot.
Today, the number of AIC member sites implementing the Ethos solution and sharing protocols and practices has grown to nearly 30 worldwide. The collaboration and research among members, which includes technology evaluations, pilot studies, and plans for clinical trials, has led to more than 30 abstracts for posters and presentations being accepted to ESTRO, AAPM, and ASTRO in 2020.
Here, we talk with members of the AIC to hear about their experiences with this collaborative effort, to learn how their research has progressed and how they’re currently using Ethos for adaptive radiotherapy in their clinics.
Herlev Hospital, Herlev, Denmark
Medisch Spectrum Twente (MST), Enschede, Netherlands
Royal North Shore Hospital, Sydney, Australia
Icon Cancer Centre – Wahroonga, NSW, Australia
Washington University, St. Louis, Missouri
The University of California, San Diego
Herlev Hospital, Herlev, Denmark
The radiotherapy division of the oncology department at Herlev Hospital in Herlev, Denmark, was the first to adopt Ethos and has collaborated with several other groups on research projects, including Washington University in St. Louis, Missouri and Royal North Shore Hospital in Sydney, Australia.
Over the past year, medical physicist Patrik Sibolt and deputy chief physicist David Sjöström have had seven abstracts accepted by ASTRO, ESTRO, and AAPM, and given numerous presentations on the hospital’s experiences treating the first patients in the world with Ethos therapy.
“We’ve treated about 14 bladder cancer patients on Ethos so far, and that has been where we’ve focused our research,” Sibolt said. “In addition to studying system feasibility and clinical results, we’ve also studied the dosimetric impact of adapting on a daily basis for bladder cancer patients. We concluded that by adapting, we can eliminate some of the margins and based on the data we’ve gathered, this represents a median reduction in high-dose treatment volume of 47 percent. That’s very promising news.” 1, 2
The Herlev team has also focused on technical aspects of the system, studying the feasibility of using adaptive radiotherapy for other disease sites, such as prostate, and the workflow, and the QA processes required for these adaptive treatment plans.
“Our studies have concluded that the Ethos system is exceptionally fast and that the AI-generated structures needed no—or only minor—editing in most cases,” Sibolt said. “For the first 100 adaptive fractions, we had median session durations of 12.5 minutes, well within our standard treatment time slots.” 3
Currently, Sjöström and Sibolt are working with other consortium members to design clinical trials—one for bladder cancer and another for anal cancer—to show the clinical impact in toxicity reduction.
“The collaboration side is what excites me the most,” Sibolt adds. “We’ve studied a lot of aspects, from risk analysis with Royal North Shore, to QA to validate the independent dose calculation system, to working on providing the community with guidelines on how to implement specific techniques. Our research covers a broad spectrum and we have the potential to broaden it even more with more partners in the consortium.”
Medisch Spectrum Twente (MST), Enschede, Netherlands

For Erik van Dieren, medical physicist at the Medisch Spectrum Twente (MST) community hospital in Enschede, in the eastern region of The Netherlands, being able to contact other consortium members like Sjöström and Sibolt at Herlev was extremely helpful in understanding how to proceed, what’s feasible, and the rationale behind certain decisions. MST treats about 2,500 patients a year and in December 2019, decided to convert its Halcyon system to Ethos and implement the adaptive workflow for prostate cancer patients.
“We understood it was a grand undertaking, especially being only the second user and a small facility,” van Dieren said. “But Ethos fits all needs. We’re able to treat three cases an hour on Ethos with the adaptive workflow and about 40 patients a day using the IGRT workflow. We’re currently looking at ways to expand to treat other pelvic tumors and tumor groups, including thorax.”
MST began its research on adaptive radiotherapy treatment for prostate cancer, studying hypofractionation and margin reduction based on its current adaptive treatments. Its abstract, Adaptive radiotherapy can be applied routinely, using an artificial intelligence solution, to treat prostate cancer patients, was accepted for digital poster presentation at ASTRO this year.4
Meanwhile, Lisanne Zwart, a technical physician at MST, has been assisting with a lung study, building a database of 280 patients with daily and weekly CBCT imaging, and evaluating contour and plan generation in the Ethos emulator.
“The study showed that adaptive radiotherapy is feasible for lung cancer treatment—adaptive plans were created within a reasonable time, and chosen for nearly all fractions,” Zwart said. “We’re currently investigating the feasibility of reducing target volume.”5
The abstract, Improved treatment quality in stage III lung cancer patients using online adaptive radiotherapy in a simulation setting, also has been approved for digital poster presentation at this year’s virtual ASTRO meeting.
Royal North Shore Hospital, Sydney, Australia
Royal North Shore Hospital in Sydney, Australia, also is a small, state-funded facility that treats about 1,500 cancer patients a year. It was the third facility to implement an Ethos system and Jeremy Booth, head of medical physics, was keen to get involved with the AIC to share research and experiences. Currently, the hospital is adapting treatments for rectum and head and neck cancers, and developing protocols to use the adaptive workflow for multiple sites, starting with cervix, bladder, prostate, prostate bed. It’s also evaluating the system for simulation-free palliative treatment.
While preparing for broad use of Ethos for adaptive, Booth has been working in close collaboration with Herlev Hospital and Washington University, including joint research on the abstract for AAPM, Towards quality assurance for first AI-driven online adaptive radiotherapy based on Failure Mode and Effect Analysis (FMEA). The poster reports on the study, which assessed the AI-driven adaptive system for risk toward development of a quality assurance program that gives the international community a platform from which to safely implement the system in their clinics.6
“Our experience of being part of AIC has been excellent—the group is very cordial and open, and we’ve moved from supporting each other in implementing systems to more research collaboration,” Booth said. “It’s enabled us to target the research in areas where more work needs to be done and not to repeat too much the work of others.”
Booth and his team are also investigating other aspects of adaptive radiotherapy, including its online use as a replacement for simulation-based radiation therapy and toward combining online with real-time adaptation for patient motion.
“Our research is not just about shrinking margins, for which we are involved in planning three trials, but it’s also about patient comfort and minimizing the number of visits for patients who are in pain,” Booth said. “Bringing them straight to Ethos, planning, and then treating them is one less of two visits and a dramatic improvement in workflow for that group of patients.”
Icon Cancer Centre – Wahroonga, NSW, Australia
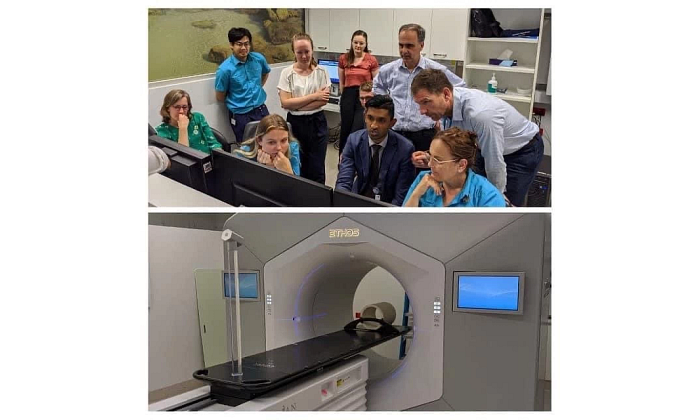
![]()
Icon Group operates 25 radiation oncology centers across Australia and New Zealand, and one radiation oncology center in China, with several currently in development. Icon were the first in the southern hemisphere to treat on an Ethos system using Adaptive Intelligence and are set to install a second Ethos system in one of their Australian centers by early 2021. Icon uses Ethos in both online adaptive mode and in its more conventional IGRT mode. So far, the online adaptive workflow is used for prostate cancer patients, but the group is looking to explore other disease sites as experience and the body of evidence grows.
The Icon team is also interested in studying many other areas of adaptive radiotherapy and has conducted several technical studies looking at the workflow and accuracy of QA tools. More recently, they have also embarked on a set of planned clinical studies as part of cross-consortium collaboration.
“The consortium provides a mechanism to easily communicate with other early adopters of this technology, to learn from their experiences, validate our findings, and to consider alternate workflows—especially since our respective roles are different depending on which part of the world we are from,” said Trent Aland, national director of medical physics at Icon. “It is this collaborative work that, once combined and finalized, will be available to all Ethos users to help them implement this technology efficiently and safely.”
Prior to Ethos, Icon had no efficient way of adapting treatments to account for daily changes in patient anatomy, but now clinicians can choose to treat a particular fraction based on the original treatment plan or based on a plan that is created to match the patient’s anatomy on the day of treatment.
“To date, online adaptive radiotherapy has only been possible in centers with the resources and technology required to effectively customize a patient’s treatment while that patient is on the couch,” Aland said. “Ethos changes this for centers large and small anywhere in the world, and this, in turn, will benefit patients, and provide them with access to the life-changing technology, closer to their homes.”
Washington University, St. Louis, Missouri
In addition to the work of the centers mentioned above, other clinics and university institutions had abstracts accepted for publication. Washington University has collaborated with Herlev and Royal North Shore on two abstracts, in addition to having five additional abstracts accepted for its own research on Ethos. The abstract, Validation of an AI-Driven Treatment Planning System for Adaptive Radiotherapy, concluded that the treatment planning feature of the Ethos system calculates dose accurately and that the system operates in a manner that is consistent and safe for clinical use.7
The University of California, San Diego

The University of California San Diego (UCSD), in La Jolla, California, had three abstracts accepted and published for AAPM examining the use of Ethos in daily online adaptations. From this research, the UCSD team has concluded that online daily adaptation using Ethos can double the fractions of prostate treatments where CTV Dmin>=95% suggesting the Ethos daily adaptive workflow is superior to existing non-adapted workflows even without expert contour review/correction.8
In another UCSD study, initial results show that the fully automated Ethos IOE generated clinically equivalent plans to existing knowledge-based models that have been in routine clinical use and validated across hundreds of patients.9
UCSD’s third abstract, Can Daily Online Adaptive Therapy Overcome Prostate Patients' Periodic Non-Adherence to Full Bladder/Empty-Rectum Protocols? concludes that daily adaptive therapy can improve tumor coverage and rectal sparing, even when patients fail to adhere to full bladder/empty-rectum protocols in any given fraction.10
“Because Ethos enables automation at every stage of the treatment process, we are focused on exploiting its capabilities to re-engineer clinical workflows around increased quality and efficiency,” said Kevin Moore, deputy director of medical physics at UCSD. “We are particularly excited at the possibilities of scaling up online adaptive radiotherapy so that we can demonstrate the benefit to patients. To that end, we are actively pursuing a multi-institutional clinical trial within the consortium to use daily online adaptation as the intervention to reduce gastrointestinal toxicity in cervical cancer.”
“The response to adaptive radiotherapy and to Ethos from the radiation oncology community has been unprecedented,” said Sasa Mutic, senior vice president of radiation treatment solutions at Varian. “As more clinics have joined the consortium, the momentum around sharing knowledge and collaboration research continues to grow. We’re confident these efforts will help remove the barriers to adaptive radiotherapy for more clinics, and make personalized, flexible treatment strategies more accessible than ever to patients globally.”
The information captured herein represents the genuine experience of the attributed individuals and may not necessarily represent the views of Varian or the above-referenced institution. Individuals were not compensated for their participation. Radiation treatment may not be appropriate for all cancers. Individual results may vary.
Notes:
1 Sibolt P, Andersson L, Calmels L, et al. Results of a pilot study on online adaptive radiotherapy of bladder cancer with artificial intelligence-driven full re-optimization on the anatomy of the day. American Society for Radiation Oncology. Online. 2020.
2 Andersson L, Behrens CF, Calmels L et al. First clinical experience of online adaptive radiotherapy driven by CBCT and artificial intelligence. European Society for Radiotherapy and Oncology. Online. 2020.
3 Andersson L, Calmels L, Sibolt P et al. Evaluation of an artificial intelligence driven planning system for online adaptive radiotherapy. European Society for Radiotherapy and Oncology. Online. 2020.
4 Van Dieren EB, Zwart LGM, Bhawanie A et al. Adaptive Radiotherapy Can Be Applied Routinely, Using an Artificial Intelligence Solution, to Treat Prostate Cancer Patients. American Society for Radiation Oncology. Online. 2020.
5 Zwart LGM, Woutersen D, ten Asbroek L et al. Improved Treatment Quality in Stage III Lung Cancer Patients Using Online Adaptive Radiotherapy in a Simulation Setting. American Society for Radiation Oncology. Online. 2020.
6 Booth J, Sibolt P, Laugeman E et al. Towards Quality Assurance for First AI-Driven Online Adaptive Radiotherapy Based on Failure Mode and Effect Analysis. Joint Meeting of the American Association of Medical Physics and the Canadian Organization of Medical Physics. Vancouver, BC, Canada. Online. 2020.
7 Pryser E, Cai B, Reynoso F et al. Validation of an AI-Driven Treatment Planning System for Adaptive Radiotherapy. Joint Meeting of the American Association of Medical Physics and the Canadian Organization of Medical Physics. Vancouver, BC, Canada. Online. 2020.
8 Moazzezi M, Moore K, Kisling K et al. To Tweak Or Not to Tweak? Prospects for Daily Online Adaptation Using Unedited CBCT Auto-Segmentation. Joint Meeting of the American Association of Medical Physics and the Canadian Organization of Medical Physics. Vancouver, BC, Canada. Online. 2020.
9 Ray X, Moazzezi N, Bojechko C et al. Evaluation of a Novel AI-Driven Automated Treatment Planning System. Joint Meeting of the American Association of Medical Physics and the Canadian Organization of Medical Physics. Vancouver, BC, Canada. Online. 2020.
10 Moazzezi M, Moore K, Kisling K et al. Can Daily Online Adaptive Therapy Overcome Prostate Patients' Periodic Non-Adherence to Full Bladder/Empty-Rectum Protocols? Joint Meeting of the American Association of Medical Physics and the Canadian Organization of Medical Physics. Vancouver, BC, Canada. Online. 2020.
