Earlier this year, Varian received 510(k) clearance from the U.S. Food and Drug Administration (FDA) for TrueBeam and Edge radiotherapy systems featuring the optional HyperSight imaging solution. HyperSight imaging can now be used to help enhance the quality of radiotherapy treatments across the entire Varian portfolio of linear accelerators (linacs).*
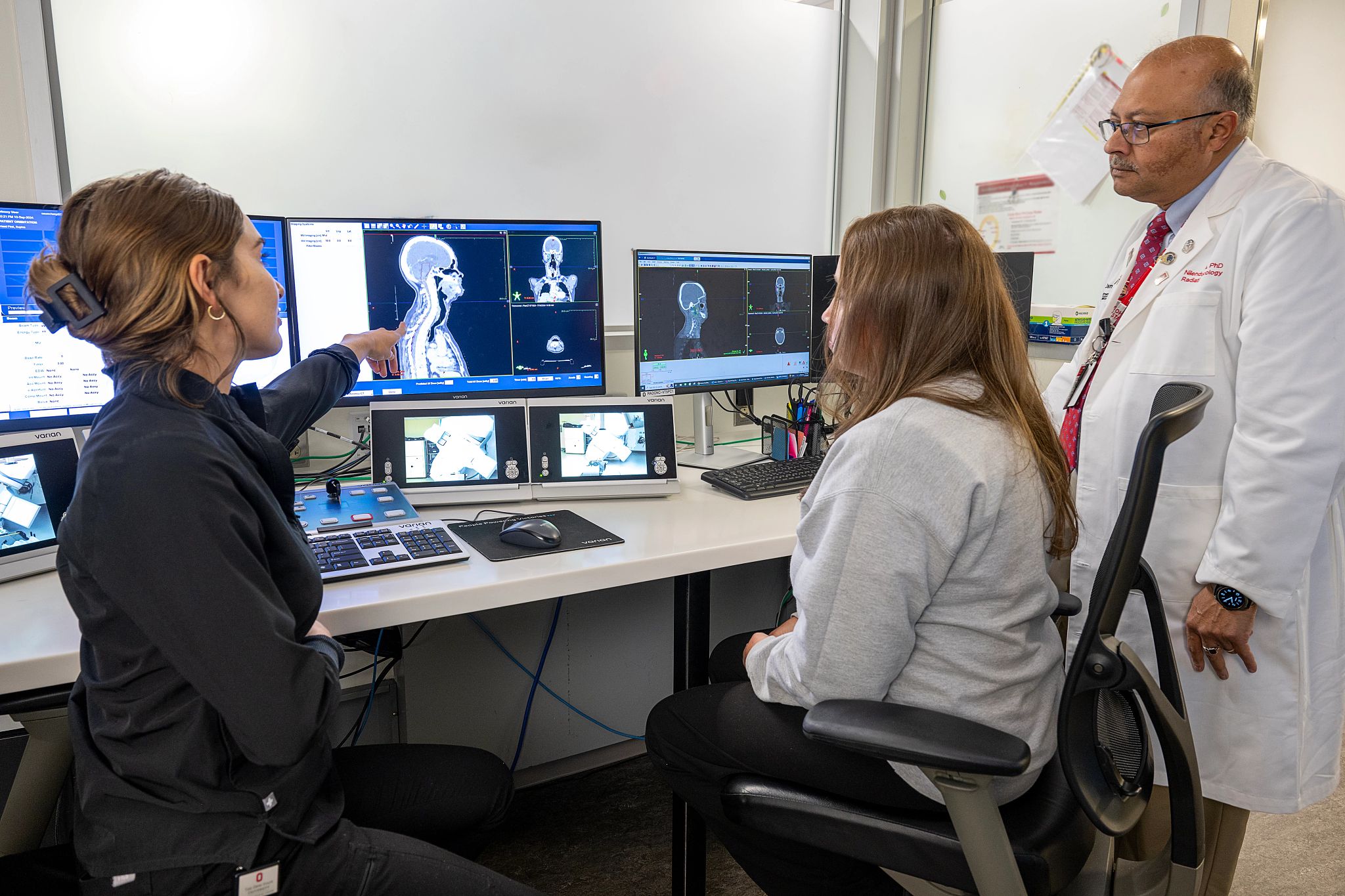
When adopting new technology, such as HyperSight imaging, radiation therapy departments weigh two primary concerns—the advancement of patient care and the effect on clinic workflow and efficiency. Clinicians from two leading U.S. cancer centers now using HyperSight on TrueBeam and Edge systems ̶ The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC–James) in Columbus, Ohio, and the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC) in Baltimore, Maryland ̶ shared their clinical experiences with HyperSight, as well as their observations about the ways it can serve to enhance patient care.
Increased Hounsfield Unit accuracy
In addition to 10 beam-matched platforms in clinical use, the OSUCCC – James operates one TrueBeam dedicated to education and research, where HyperSight was initially evaluated. The imaging solution has since been deployed for clinical use on a TrueBeam and on two Edge systems, with another Edge system installation scheduled for late 2024.
“Evaluating patient images is often qualitative. Someone looks at the image and says, ‘Does it look better?’ As physicists, we want more quantitative data,” said Nilendu Gupta, PhD, FAAPM, Vice Chair and Chief of Medical Physics at the OSUCCC–James. “We performed a series of quantitative tests comparing HyperSight images to traditional CBCT images and have some great data to show that there are quantitative advantages to HyperSight, such as the ability to better distinguish objects of different densities, to remove imaging artifacts from metallic objects, and to visualize a larger field of view.”
With HyperSight on TrueBeam and Edge systems, the potential for offline adaptive planning is expected to change due to what Dr. Gupta characterizes as an otherwise “challenging workflow” whenever anatomy and tumor changes are detected during the course of treatment.
“We see a large volume of patients today, especially for head & neck and breast cancer treatment, where with daily imaging we start seeing changes in anatomy or in tumor size and shape. Right now, adaptation to these changes presents a challenging workflow. Do we decide, based on a poor-quality cone-beam CT image, that the change is significant enough to go through the whole planning process again?”
To answer this type of question, a study sponsored by Varian is being launched at the OSUCCC–James to look at the dose calculation accuracy of HyperSight images for use in offline plan adaptation, as one of its objectives. “From our dosimetric studies with phantoms in our non-clinical environment, we have seen the image quality necessary to perform plan adaptations. However, we haven’t used HyperSight images to adapt plans for patients yet; that will be investigated in our study,” reports Dr. Gupta. “We are hopeful that HyperSight will help us create a more efficient workflow for offline adaptive planning, where we can use today’s image to re-plan a treatment for tomorrow, if warranted.”
At UMGCCC, where HyperSight has been used clinically for several months, Amit Sawant, PhD, Vice Chair for Medical Physics, concurs that the improved quality of in-room imaging has the potential to enhance patient care. The HyperSight CBCT image quality approaches that of CT simulation, enabling patients to be positioned accurately and with more confidence, he said, adding that it also clearly shows changes in the anatomy over the course of treatment. “We strongly suspect that the quality and accuracy of the HyperSight CBCT images are high enough to use for adapting the treatment,” Dr. Sawant said, which will enable greater personalization of treatment to better meet the physician’s intent for each patient. UMGCCC is currently conducting a prospective clinical trial in cancer patients to assess whether plan adaptation using HyperSight cone-beam CT imaging is clinically acceptable.
“Directly using HyperSight CBCT images acquired on the linac for accurate dose calculations would be a significant time saver, especially in busy centers with fully utilized CT scanners,” said Jochen Cammin, PhD, Assistant Professor, University of Maryland School of Medicine.
Reducing artifacts
A quantitative advantage of HyperSight for patient care at the OSUCCC–James is the reduction in metal artifacts in the images, Dr. Gupta shared. CT systems used for simulations can reduce distortions created by metal implants, but in-room cone-beam CT imaging systems have not had the same capability. “Metal artifacts are a challenge we have, especially on the systems we use for stereotactic treatments,” he added.
“It is difficult to visualize what you have planned and where you are delivering treatments if the patient has metal implants near the target that impact the quality of imaging,” Dr. Gupta explains. “With HyperSight, we have obtained patient images that clearly show the metal artifact reduction.”
For this reason, two Edge systems at OSUCCC–James were the first to be upgraded to HyperSight. And the study mentioned above will also gather more data on artifact reduction and other HyperSight capabilities.

Expanding the field of view
Clinicians at both centers also mentioned the HyperSight solution’s extended field of view as another feature benefiting their clinical practice. “With the larger field of view in both axial and transverse planes, we can see more of the anatomy that we are trying to treat. Not having to reposition the patient and rescan when something falls outside the field of view of current-generation CBCT images is a huge benefit to staff and patients,” said Dr. Cammin, sharing an example of a patient with large lateral target in the shoulder. “We could not see the entire target on older CBCT images, but with HyperSight and the extended field of view, we were able to see the whole target, and that overall gives more confidence in lining up the patient accurately.”
Seeing the whole target is essential for having confidence in the patient's alignment when treating a tumor more aggressively with reduced margins, according to Dr. Gupta. “Many of our treatment volumes, especially in head & neck cases, exceed the volume of imaging we can do with the traditional imager on the TrueBeam system,” he said. Consequently, multiple images would have to be taken and stitched together at the TrueBeam console. In contrast, HyperSight captures the entire treatment volume in a single image for most of these cases."
Impact on clinical workflow
The physics experts featured here agree that HyperSight offers advantages for patient care. But what about the other concern, the impact on workflow and efficiency? “Our pre-upgrade evaluation and early clinical use indicate that HyperSight enhances patient care. HyperSight has also been a workflow enhancement for both physicians and the therapists who treat at the machine,” Dr. Gupta said.
Tessa Rodgers and Sabrina Mooney, lead radiation therapists at the OSUCCC – James who have been using HyperSight on Edge systems for a few months, concur. While the user interface has not changed significantly with the upgrade, the larger field of view and speed of acquisition have made a difference for therapists and patients. "HyperSight has given our team the ability to treat off one single, comprehensive image. Previously, multiple images were required for many of our H&N and GYN patients. HyperSight has saved these patients time on the treatment table and lessened the imaging dose they receive," said Rodgers. "For the therapy team, it has been beneficial for simplifying our imaging workflow and successfully completing appointments within their scheduled timeframes."
Clinical implementation of HyperSight imaging for adaptive planning decisions will be the next step, reports Mooney. “Using HyperSight imaging for adaptive planning decisions, especially with our H&N population who often face setup challenges due to weight loss and soft tissue changes during treatment, appears promising. Similarly, the possibility of CBCT-based replans is encouraging. Improved imaging protocols that enhance image quality will also aid in more accurately aligning traditionally challenging treatment sites, such as the liver.”
“Metal artifact reduction, larger field of view, and the HU accuracy for calculating dose distribution and treatment planning are HyperSight capabilities that we believe will have a significant impact on how we practice radiation therapy in the clinic,” Dr. Sawant said. Furthermore, “with HyperSight on TrueBeam, operationally nothing changes,” Dr. Cammin added. “It is giving us new capabilities without changing the way we operate. That’s very, very powerful.”
Learn more:
- Register for our webinar: TrueBeam with HyperSight Imaging Solution- The Ohio State Experience
- The HyperSight Imaging Solution: A Revolution in Resolution for Single-Bunker Sites
*Not available on the VitalBeam system.
The information captured herein represents the genuine experience of the attributed individuals and may not necessarily represent the views of Varian or the above-referenced institution.
This article is not intended as an endorsement by The Ohio State University or The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute of any particular product or device.